Monday May 6, 2024
Why Do Nurses Quit? Hint: It’s Not Burnout
BY ERIC M. PARMENTER, PH.D., MBA, CEBS, SPHR
Originally published in the Spring 2024 issue of HR Pulse magazine.

Shortage of nurses in the U.S. reached crisis proportions in 2021.1 A recent survey of 1,205 nurses employed primarily in acute care hospitals in the U.S. in 34 states sought to find out what predicted nurse job embeddedness, defined as nurses who have no plans to leave their current job.2
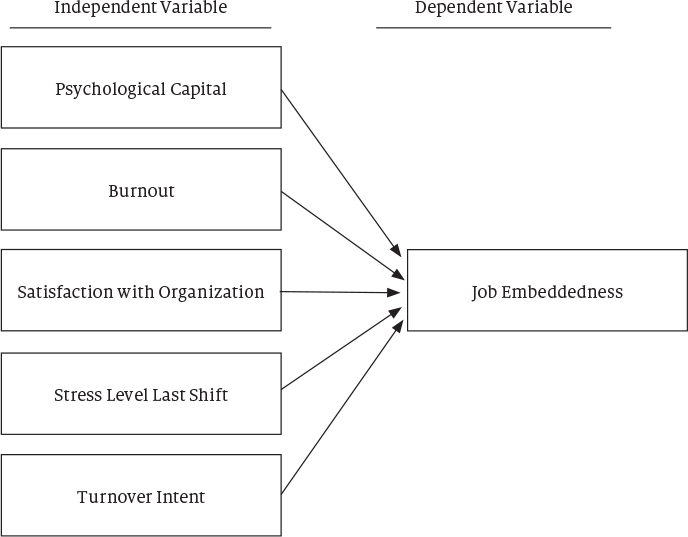
Five inputs were evaluated as contributing forces to job embeddedness, including psychological capital, burnout, a high-stress job shift, satisfaction with the organization and turnover intent.2
Background
The shortage of nurses working in hospitals is a significant and growing concern. It is important to understand what predicts job embeddedness in nursing so that nurse leaders and hospital executives can develop and implement effective workforce strategies to retain nurses in the organization.
Approximately 100,000 nurses left the workforce during the Covid-19 pandemic. According to results of a study released in 2023, another 800,000 nurses stated their intention to leave the workforce by 2027.3 Altogether, these numbers equate to one-fifth of the 4.2 million nurses in the workforce today.3 This alarming statistic underscores the need to focus on how to increase job embeddedness for the purpose of retaining nursing staff who may consider leaving the organization or the profession.
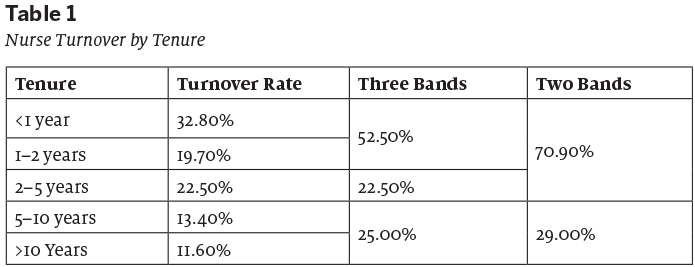
Nurse turnover: The crucial first five years
Turnover is higher for nurses in the early stages of the profession than it is for those who are more experienced. Nearly a third (32.8%) of all new hires leave within a year. Over half (52.5 %) of the departing nurses had less than two years of experience. The highest level of turnover is for nurses in their first five years (75%), whereas is much lower for those who have reached five to 10 years (13.4%) or 10 or more years (11.6%). Table 1 provides a detailed breakdown of nurse turnover rates by tenure.1
There are several factors contributing to high turnover, ranging from burnout4 to sociodemographic factors, including pay and benefits, the relationship between nurses and their boss, the nature of the job and the perception of the organization.5
Definitions of factors that contribute to job embeddedness
Job embeddedness is defined as the extent to which an employee feels they cannot leave their current job due to on-the-job and off-the-job forces involving links (how an individual is connected to other people and activities), fit (how an individual’s work relates to their values and goals) and sacrifice (the level of disruption an individual would experience if they were to quit their job).6
Psychological capital is based on four underlying constructs of hope, efficacy, resilience and optimism. These components make up the acronym H.E.R.O. and have come to be called the “HERO within.” The HERO acronym can also describe the often-heroic work that nurses perform in caring for patients under stressful conditions.7 Psychological Capital (PsyCap) has been demonstrated to improve job performance across multiple dimensions, such as job satisfaction, organizational commitment and organizational citizenship behaviors.8
Burnout in this survey was measured by the conservation of resources (COR) theory. This theory begins with the tenet that individuals strive to obtain, retain, foster and protect those things they centrally value. According to COR theory, when people’s resources are stretched or exhausted, they enter a defensive mode to preserve the self, which is often aggressive and may become irrational.9 This exhaustion, or burnout, experienced by many nurses can trigger this mode.
Finally, the peak-end rule is a bias in which people tend to remember an experience in terms of its most intense point and its end, as opposed to the sum, the duration or the average moment of the experience.10 For instance, a study found that participants rated a wonderful life that ended suddenly as better than one with the addition of mildly pleasant years. The researchers termed this the “James Dean effect.”11
Figure 1 shows how each of these variables aligns to contribute to job embeddedness, which is the goal in nursing jobs.
Population and sample
There were 1,205 participants in this sample. Of those who provided an answer or did not choose “other,” 91.4% were women, and 8.5% were men. For those who provided an answer on educational degree, those with a BSN represented 62.1% of the sample, followed by ADN at 18.5%, MSN at 13.8%, and doctorate level at 0.3%. Non-supervisors represented 84.4% of the sample, those without second jobs represented 83.9%, and day-shift workers represented 79.8%.2
Conclusion of results
This study found, using hierarchical regression analysis, the variables predicting job embeddedness were job satisfaction (explaining 30% of the variance), intention to leave the organization in six months, (explaining 8% of the variance), and PsyCap (explaining 2% of the variance). In total, this model accounts for 40% of the variance in job embeddedness. Perhaps what is most interesting is that burnout and a recent stressful job shift did not emerge as predictors of job embeddedness.2
Interpretation of findings
The goal of healthcare organizations that employ nurses is to attract, retain and engage their nursing staff. While job embeddedness has been described as “stuckness,” it can be thought of as stuck in a good way because it has consistently been shown to be associated with positive workplace behaviors.12 Over time, higher levels of job embeddedness contribute to increased proactivity and have a contagious impact on reducing the turnover intentions of coworkers.12, 13
If organizations employing nurses wish to increase job embeddedness, emphasizing PsyCap will be beneficial, especially if incorporated into the organization’s culture and career development efforts. During the Covid-19 pandemic, the rise of a volatile, uncertain, complex and ambiguous environment (VUCA) has contributed to an increase in anxiety, depression and other mental health concerns. PsyCap can be used as a realistic alternative and positive alternative.8 This will help improve the nurses’ overall satisfaction with the organization.
The most important variable in this study is the satisfaction of the nurse with their employer as an organization, the most significant predictor accounting for 30% of the variance in job embeddedness. The following recommendations are derived from the findings of this study.
Recommendations
Three recommendations to increase nurses’ job embeddedness can be derived from this study’s findings. First, PsyCap training and support can be layered into learning and development programs as part of overall career development. PsyCap serves as a predictive variable of job embeddedness, and the theoretical basis demonstrates that higher levels of PsyCap make a difference across various job performance and retention dimensions.
Second, focusing on the organization’s caring, supportive culture is central. This involves integrating career building into the broader cultural initiatives and creating a leader-led line-of-sight into the organization’s mission, vision and values. This approach directly leads to increased satisfaction with the organization, which is the most salient factor in job embeddedness.
Building an organization where nurses experience a sense of pride and belonging promises to produce greater job embeddedness. The nurse’s satisfaction with the organization encompasses all other factors. A good culture is the essence of strong organizational satisfaction. Culture serves as the great melting pot that incorporates all other factors. Culture starts with leadership at the top of the organization. A study by Hashish revealed positive and significant correlations between nurses’ perception of the overall ethical work climate and each aspect of perceived organizational support, commitment, as well as job satisfaction.14 Ethics are at the heart of leadership, leadership is at the heart of culture, culture is at the heart of nurses’ satisfaction with the organization, and nurses’ satisfaction with the organization is at the heart of job embeddedness.
Third, offer healthcare navigation as part of the employee benefits plan. Nurses spend so much time and energy caring for others that they neglect caring for themselves. While many employers offer wonderful benefits, including support with mental and behavioral health, employees often do not take advantage of these programs because benefits are complex and confusing. That is where care navigation plays a role, serving as a white-glove concierge support for employees, providing a single point of contact for everything related to benefits.
For instance, consider an employee who has received a new diagnosis, perhaps for something serious like cancer. Navigating through the process of finding the right healthcare providers and managing multiple medical bills, especially overwhelming at a time when the employee may be experiencing great anxiety. Understanding health benefits alone can be confusing. Healthcare navigation can help with all these issues, including connecting the employee to mental health resources, often for free.
Other examples include connecting members with employee assistance programs (EAPs) that offer several free counseling visits, so the member doesn’t have to meet a deductible first.
Offering healthcare navigation along with other benefits can demonstrate an employer’s commitment to establishing a culture of caring. This commitment, in turn, can enhance job embeddedness, where employees choose to stay in their job because the value of staying outweighs the value of leaving. Healthcare navigation is a great way to increase the overall satisfaction level that employees have with their employer.
Finally, valuable insights can be learned from the findings that were not confirmed. The discovery that burnout and a recent high-stress job shift are not predictive of job embeddedness might be surprising. While popular press and academic literature often discuss burnout as a precursor to turnover, this study did not find a predictive relationship between burnout or a high-stress recent shift and job embeddedness in the final model. Nevertheless, it is important to note that burnout does influence job embeddedness in a more specific, direct sense. Overall satisfaction with the organization, however, emerges as a significant variable in predicting job embeddedness.
Eric Parmenter is the vice president of hospitals and health systems for Quantum Health. He is established as a national expert on employee benefits, behavioral economics and psychology. A consultant with deep experience in health plan strategy, design, prevention care, and productivity and behavioral economics, Eric is a seasoned health tech executive.
References
- 1. Nursing Solutions, Inc. (2023). 2023 NSI National Health Care Retention and RN Staffing Report. https://www.nsinursingsolutions.com/Documents/Library/NSI_National_Health_Care_Retention_Report.pdf
2. Parmenter, E. (2023). I Had a Bad Day but Tomorrow I Will Carry On: Nurse Burnout and the Relationship Between Psychological Capital and Job Embeddedness (Doctoral dissertation, The Chicago School of Professional Psychology).
3. NCSBN Research Projects Significant Nursing Workforce Shortages and Crisis. (2023). PR Newswire Association LLC. https://www.ncsbn.org/news/ncsbn-research-projects-significant-nursing-workforce-shortages-and-crisis
4. Dzau, V. J., Kirch, D., & Nasca, T. (2020). Preventing a Parallel Pandemic — A National Strategy to Protect Clinicians’ Well-Being. The New England Journal of Medicine, 383(6), 513–515. https://doi.org/10.1056/NEJMp2011027
5. Halter, M., Boiko, O., Pelone, F., Beighton, C., Harris, R., Gale, J., Gourlay, S., Drennan, V. (2017). The determinants and consequences of adult nursing staff turnover: a systematic review of systematic reviews. BMC health services research, 17(1), 1–20.
6. Crossley, C. D., Bennett, R. J., Jex, S. M., & Burnfield, J. L. (2011). “Development of a global measure of job embeddedness and integration into a traditional model of voluntary turnover”: Clarification to Crossley et al. (2007). Journal of Applied Psychology, 96(6), 1316–1316. https://doi.org/10.1037/a0025569
7. Mohammed, S., Peter, E., Killackey, T., & Maciver, J. (2021). The “nurse as hero” discourse in the COVID-19 pandemic: A poststructural discourse analysis. International Journal of Nursing Studies, 117, 103887–103887. https://doi.org/10.1016/j.ijnurstu.2021.103887
8. Luthans, F., & Broad, J. D. (2022). Positive psychological capital to help combat the mental health fallout from the pandemic and VUCA environment. Organizational Dynamics, 51(2), 100817–100817. https://doi.org/10.1016/j.orgdyn.2020.100817
9. Hobfoll, S. E., Halbesleben, J., Neveu, J.-P., & Westman, M. (2018). Conservation of Resources in the Organizational Context: The Reality of Resources and Their Consequences. Annual Review of Organizational Psychology and Organizational Behavior, 5(1), 103–128. https://doi.org/10.1146/annurev-orgpsych-032117–104640
10. Kahneman, D. (2011). Thinking, fast and slow (1st ed.). Farrar, Straus and Giroux.
11. Diener, E., Wirtz, D., & Oishi, S. (2001). End Effects of Rated Life Quality: The James Dean Effect. Psychological Science, 12(2), 124–128. https://doi.org/10.1111/1467–9280.00321
12. Li, J. J., Mitchell, T. R., Lee, T. W., Eberly, M. B., & Shi, L. (2022). Embeddedness and perceived oneness: Examining the effects of job embeddedness and its trajectory on employee proactivity via an identification perspective. Journal of Applied Psychology, 107(6), 1020–1030. https://doi.org/10.1037/apl0000961
13. Felps, W., Mitchell, T. R., Herman, D. R., Lee, T. W., Holtom, B. C., & Harman, W. S. (2009). Turnover Contagion: How Coworkers’ Job Embeddedness and Job Search Behaviors Influence Quitting. Academy of Management Journal, 52(3), 545–561. https://doi.org/10.5465/AMJ.2009.41331075
14. Hashish, A. (2017). Relationship between ethical work climate and nurses’ perception of organizational support, commitment, job satisfaction and turnover intent. Nursing Ethics, 24(2), 151–166. https://doi.org/10.1177/0969733015594667
Originally published in the Spring 2024 issue of HR Pulse magazine.

